Health data and its imagined uses have been an exciting topic lately, with artificial intelligence projects aiming to identify missed treatment opportunities, reduce readmissions, or provide more personalized care plans for patients. These are ambitious ideas that can result in significant improvements for patient care, but all share the requirement of complete and accurate data to make proper assessments.
To ensure that the information in an organization’s EHR is acceptable, proper data quality assessment (DQA) procedures must be established. A literature review published in 2013 created a framework for EHR data quality that was based on completeness, correctness, concordance, plausibility, and currency.
Researchers from Washington University in St. Louis and the Oregon Health & Science University recently extended this literature review for a JAMIA article by examining PubMed articles referring to quality assessments of EHR data over the ten-year timeframe since the original publication.
The review found 103 papers that had been published, showing an increase in papers written since the original review. Despite the wide variety of authors examining the subject, consistent dimensions were shared, although a single DQA standard didn’t emerge.
The original five elements that were considered were reaffirmed from the research alongside two new dimensions: conformance and bias. Conformance, which is defined as having compliance with a defined representational structure, appeared in 18 papers, while bias showed up in 11 papers.
Bias was defined as a dimension that indicates, “missingness not at random.” The real-world examples of this principle show that completeness of data is often influenced by one or more additional factors. There can be a difference in recording patient information when it comes to race, but also considerations like the fact that sicker patients tend to have more complete charts or using only structured or only unstructured data due to availability.
22 of the papers were categorized as “tools,” or frameworks for the actual DQA process. Four themes emerged in this area: use-case flexibility, scalability, a common data model, and automation. It seems, though, that flexibility is the standard at this point, as DQAs are occurring in a manual and one-off fashion. The priority here is making this process efficient and repeatable without making the structure too rigid.
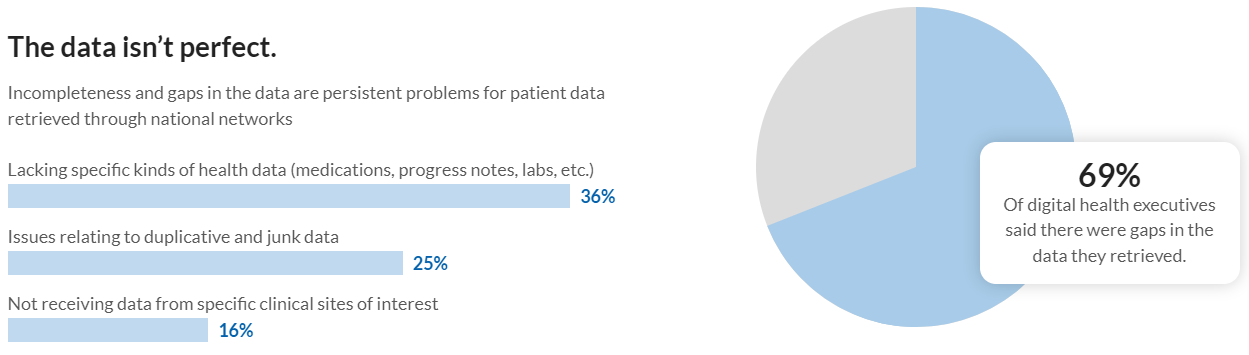
Reaching an agreement on how to assess data translates into improved outcomes at local levels and largely increased interoperability and shared resource opportunities at a national level. Considering that nearly 70% of digital health executives report gaps in data from national networks, there’s a big opportunity here.
It’s actually quite common, though, that we speak to hospital leadership and find that there isn’t a good idea of how accurately information is added to the EHR. When healthcare institutions use our software to automate their data entry, they not only increase the quantity, pace, and accuracy of their data, but they also have insight into the data’s quality to shed light on deficiencies and opportunities.
Until a healthcare organization is evaluating their data, it’s impossible to know where missed opportunities for advanced intervention, health maintenance plans, home health care, etc.
Our HealthyData software finds these valuable care insights in your incoming non-interfaced documents. Rather than calling these files “unstructured” and letting them sit in the media tab unavailable for trending or subjecting your HIM staff to unending data entry, we can:
Classify documents
Identify desired data per document type
Match to patients, orders, encounters
Send data and documents to EMR, DMS, or any other repository
Technology will be able to do wonderful things with complete and accurate repositories of healthcare data. If you’re struggling to staff your data entry roles, believe some of that staff might be better suited for other tasks, or just want better data faster, send us a message and we’ll show you the type of difference automation can make at your healthcare organization.
About the Author: Chris Mack
Chris is a Marketing Manager at Extract with experience in product development, data analysis, and both traditional and digital marketing. Chris received his bachelor’s degree in English from Bucknell University and has an MBA from the University of Notre Dame. A passionate marketer, Chris strives to make complex ideas more accessible to those around him in a compelling way.