Preparing the Financial Case for a Project
Primarily, everything done in healthcare is directed to the benefit of the patient’s health. However, there is an undeniability behind the running of a health system. It must operate on a positive operating budget or sooner or later, it will cease to exist and cease to benefit the patient.
To that point, every project, with rare exception, requires a “payback” that is supported by a return or savings in dollars. The exceptions are those projects that might not have a clear measurable payback but are deemed necessary by organizational leadership. For those projects requiring a more tangible payback, that payback may come in the form of raised top line revenue and/or a lowered bottom line (lowered expenses); either must positively affect the operating margin. It is to the latter that this blog is directed.
There’s a continuum of ways organizations measure the impact a project will have. Some organizations may require a relatively simple financial impact statement such as:
-
Reduced FTE with automated process – Decreased manual entry (50% or greater). Reallocation of FTE, with reduction of manual entry, to other needed departmental functions/work.
Others might want an impact statement where the expected financial benefit is outlined in more detail. Incorporating all external and internal costs:
-
Tying to physician retention and lowered burnout rates. Lowered expense through higher utilization of FTEs. An impact statement for a project of this type might look something like this:
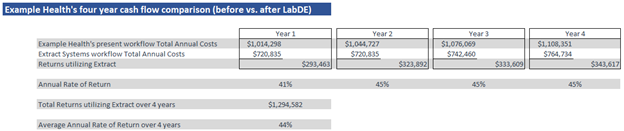
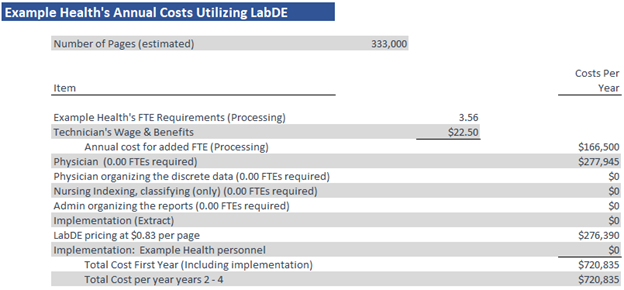
Exhibit 1
The focus of this blog is one of defining a structure and highlighting the fundamental financial and productivity building blocks of the project. The expected benefit is calculated by incorporating as many external and internal costs as can be identified. I’ll detail out the expenses that embody the subtotals in Exhibit 1.
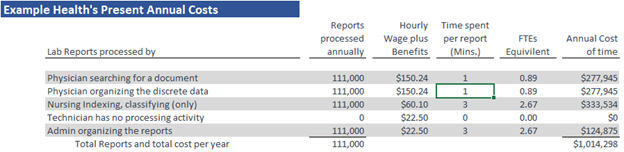
The first thing to address in building a proforma are what your present costs are, a baseline from which to measure from. In this example, we’re looking at workflow improvement. Given the “Great Resignation” currently underway, there may be an appetite within health care organizations to make the team more productive as a strategy to accommodate any staffing reductions.
The first line of Exhibit 1, “Present Total Annual Costs,” is the sum of the cost variables associated with Example Health’s current workflow for indexing and classifying documents originating from outside the health system where data interfaces don’t exist. It’s important to note that hospitals process outside documents differently. In this example, discrete data is not being abstracted into the EHR, manually or otherwise. Documents are linked in the EHR and physicians search for the resulted lab reports and review the documents themselves in search of the discrete data elements of interest.
If you’re interested in different proforma examples where different document processing workflows are in place, here are a few more examples:
-
Nursing is indexing, classifying, and abstracting from reports with physicians reviewing
-
Technicians indexing, classifying, and abstracting from reports
The variables that are utilized in each workflow are:
-
Volume of pages or documents processed annually
-
Physician workflows and time associated with the workflow
-
Nursing workflows and time associated with the workflow
-
Technician workflows and time associated with the workflow
-
Administrative Assistant workflows and time associated with the workflow
-
Other staff members’ workflows and time associated with the workflow
-
Physician average salary
-
Nursing average salary
-
Technician average salary
-
Administrative Assistant average salary
-
Other staff member average salary
-
Hours each staff member will spend participating in the implementation of the project
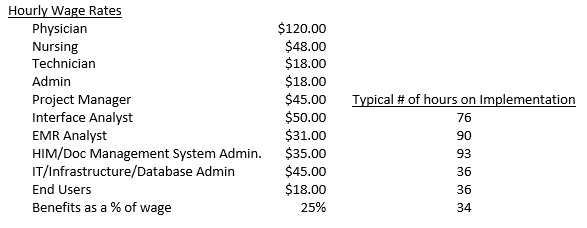
Example Health’s labor costs used:
After identifying input variables associated with the workflow and the values for each of the variables, building the present annual costs is relatively straight forward as highlighted in Exhibit 2 below.
Exhibit 2
The next step, preparing the vendor’s costs, is going to require going outside the health system to get some of the numbers. If you’re fortunate enough to be working with a sales executive that is a trusted advisor, getting the data, understanding the future workflows and associated costs, as well as verification of that data through customer references will be a relatively efficient process. If you don’t have that trusted advisor relationship, gathering the data will require more diligence on your part. One way or another, make sure that the data is verifiable.
Continuing with this example, the input variables examined post implementation don’t change. The values of the variables do:
Exhibit 3
Note that the cost of change includes both the external costs that are incurred as a result of contracting with the vendor (i.e. Implementation (Extract)) as well as internal (Implementation: Example Health personnel). The Implementation (Extract) costs are straightforward. They should be listed on the proposal coming from the vendor.
The internal costs are predicated on the hours of work each individual stakeholder will incur as part of the implementation and their associated wages/salaries. The vendor should be able to give you an idea of the former. The latter should be available through your HR department. For this example, the table above labeled “Examples Health’s labor costs:” details both.
Another note: Look for any third-party costs (one-time and annual). There are none listed in this proforma as there are none in this example. However, as part of the proforma build, you should be aware of any third-party costs that might arise. Typical third-party costs for many projects are EHR interface costs and annual maintenance fees on the interfaces.
Finally, be aware of how your leadership prefers to see proformas. In this case, because it’s an operational expenditure based investment, the format I chose to use is Rate of Return (RoR). With an operational expenditure it’s much more timely to tie the expense to the return. Return on Investment (ROI) may be the format your leadership chooses as a financial model. It’s like RoR. The primary difference is you apply Net Present Value (NPV) calculations using the Internal Rate of Return (IRR) chosen by your financial leadership.
Extract Systems’ value proposition is one of improving workflows for health system departments/areas receiving external documentation were indexing and classifying is required. Departments/areas like:
-
Hospital Information Management
-
Oncology
-
Accounts Payable
-
Ambulatory Clinics
-
Specialties
We take a step further for improving the workflows for health system departments/areas receiving external documentation where, on top of indexing and classifying, abstraction of discrete data is also needed. Departments/areas like:
-
Transplant
-
Laboratory
If you’d like to see how we can help streamline this aspect of your workflow while seeing a healthy RoR please reach out to me at:
Norm Kruse